An Electronic Eye Implant Is Helping People See Again - Here's How The Tech Works
There are a few notable tech inventions that have changed the medical industry forever. From the use of AI for disease detection to 3D printing biomedical implants and drugs, advances in modern medicine show no signs of slowing down and are finding new ways to improve people's health. A prime example of this is the PRIMA visual prosthesis, an electronic wireless retinal implant system that's helping people to see again. Clinical trial results published on October 20, 2025, in the New England Journal of Medicine, demonstrated that the device improved the eyesight of people suffering from age-related macular degeneration (AMD).
AMD causes the center of a person's vision to fade or blur, so even everyday tasks like reading or seeing faces become challenging. It affects approximately 5 million people around the world, and there's been no known treatment to bring back lost vision. The trial brought in 38 participants at 17 hospitals across France, Germany, Italy, the Netherlands, and the United Kingdom. It was led by an international team including José-Alain Sahel from the University of Pittsburgh, Daniel Palanker from Stanford University, and Frank Holz from the University of Bonn.
The participants were 60 years old or older and had significant central vision loss due to foveal atrophy. One year after surgery, over 80% of those who participated regained the ability to recognize letters, numbers, and words. Before surgery, many participants' vision was so poor that they couldn't read any letters on a standard eye chart.
The surgical procedure and system components
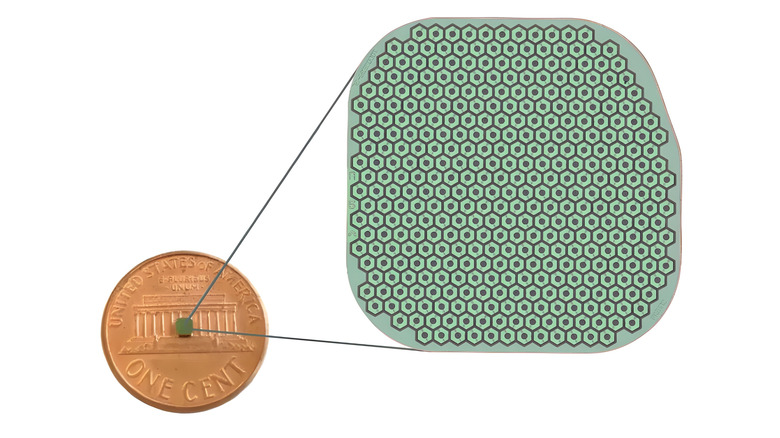
The PRIMA implant itself measures just 2mm by 2mm and is 30 micrometers thick. It has 378 photovoltaic pixels, which are tiny units that generate electricity from light, similar to a hybrid solar cell. A trained vitreoretinal surgeon can perform the surgery, which can be done in about two hours. The surgeon will begin the procedure with a vitrectomy, where they will remove the eye's vitreous gel from between the lens and retina, so a microchip can be inserted under the central retina through a small opening or "trapdoor".
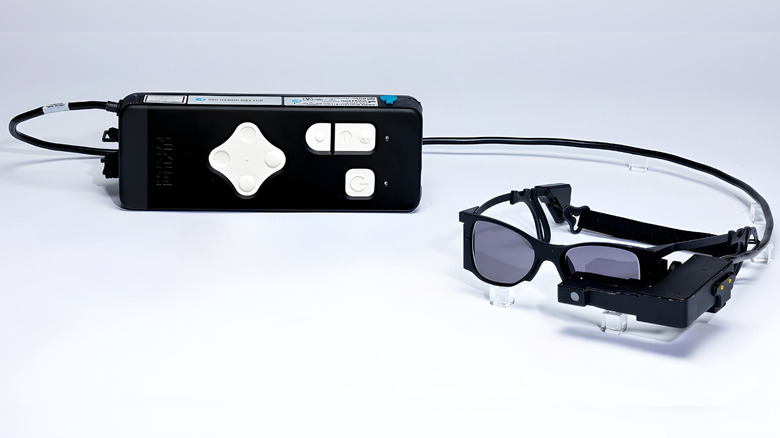
Three elements make up the entire system: a subretinal implant that converts incoming infrared light to electrical signals; augmented reality smart glasses that capture a visual scene via a camera; and a pocket-sized processor that decodes the information so the brain can learn how to interpret the signals as vision. Because the chip is photovoltaic, it only needs light to create an electric current and will operate wirelessly without needing external power cables. Four to five weeks after it's installed, patients then begin using the glasses and receive training that lasts for several months.
Patient results and future development
According to the University of Pittsburgh, the people who completed the 12-month follow-up assessments demonstrated a meaningful improvement when reading an eye chart. Of the 32 participants, 26 were able to read at least two additional lines on vision charts, using the device's digital enhancements like zoom and contrast adjustment. The average improvement was around five lines, and one participant could even read ten. The study reports that 19 participants experienced serious adverse incidents, although 95% of these were resolved quickly by spontaneous or medical intervention.
One of the participants was Sheila Irvine, who was a patient at the U.K.'s Moorfields Eye Hospital. She reported a noticeable improvement in her eyesight, saying the implant allowed her to read prescriptions, do crosswords, and read product labels. Science Corporation, the company behind the PRIMA technology, has applied for CE mark authorization in Europe and has plans to develop a next-generation device with 10,000 pixels, compared to the current 378. This is currently in its animal testing phase, as reported by Stanford Medicine.