Rice Researchers Create An Implant For Diabetics That Produces Insulin
Bioengineers at Rice University have leveraged 3D printing and smart biomaterials to create a new implant for Type 1 diabetics that produces insulin. The breakthrough is the result of a three-year partnership between researchers and the Juvenile Diabetes Research Foundation. Researchers used insulin-producing beta cells made from human stem cells to create an implant able to sense and regulate blood glucose levels by responding with the correct amount of insulin for a given time.Researchers Omid Veiseh and Jordan Miller have been working on the project for over a decade. Veiseh said that to recapitulate what the pancreas normally does requires vasculature. The pancreas has lots of blood vessels and cells that are organized in particular ways. The researchers want to print the same orientation that exists in nature.
Type 1 diabetes is an autoimmune disease causing the pancreas to stop using insulin. Insulin is a hormone required to control blood sugar levels. About 1.6 million people in America have Type 1 diabetes, and over 100 cases are diagnosed each day. The condition is managed with insulin injections, but managing insulin injections along with eating, exercise, and other activities can be difficult.
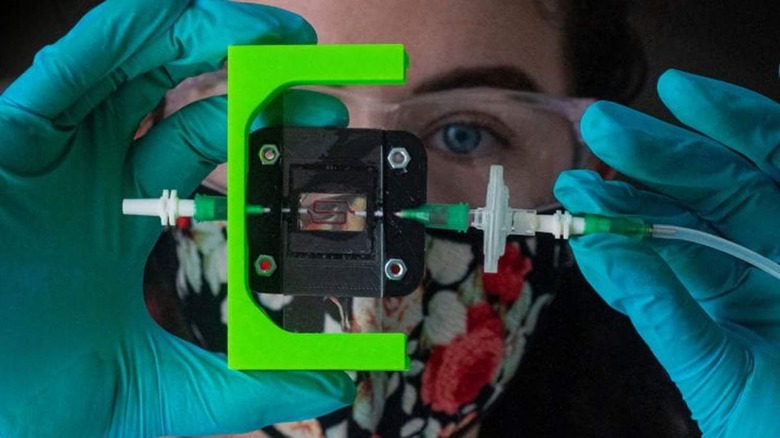
The goal of the researchers is to show that their implant can properly regulate blood glucose levels for diabetic mice for at least six months. Doing that requires them to engineer beta cells able to respond to changes in blood glucose quickly. Ideally, the insulin-producing cells would be no more than 100 microns from a blood vessel. They leveraged a combination of pre-vascularization via advanced 3D bioprinting and host-mediated vascular remodeling.
That combination gives each implant several opportunities at host integration. The cells in the implant that produce insulin will be protected with a hydrogel formulation that has been proven effective for encapsulating cell treatments in bead-sized spheres. They have pores small enough to keep cells inside from being attacked by the immune system while being large enough to allow nutrients in and insulin out of the cell.