Neurostimulation Implant Helps Stroke Patients Recover Faster
Ohio State University researchers have created a neurostimulation device that is implanted into stroke patients, helping them recover from the tragic medical event faster than traditional rehabilitation techniques. The implant, which works by stimulating the patient's vagus nerve, helps essentially rewire the patient's brain circuits, helping restore select motor functions.
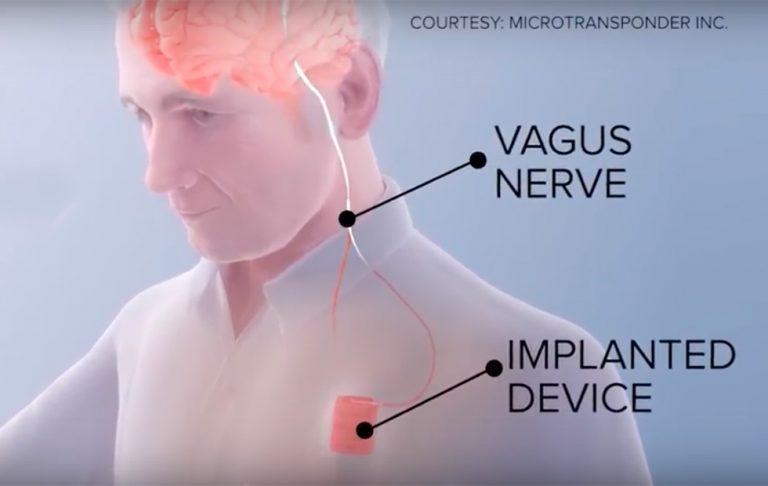
The device is called Vivistim, and it connects to the vagus nerve via an implant in the patient's chest wall (sort of like a pacemaker). Vivistim is currently undergoing a clinical trial following an earlier pilot that found about 85-percent of patients benefiting from the nerve stimulation. In traditional rehabilitative settings, it can take years for a stroke victim to regain their motor control, but the implant helps speed up that process.
Talking about the technology is OSU Wexner Medical Center's research psychiatrist Dr. Marcie Bockbrader, who said:
This nerve stimulation is like turning on a switch, making the patient's brain more receptive to therapy. The goal is to see if we can improve motor recovery in people who have what is, in effect, a brain pacemaker implanted in their body. The idea is to combine this brain pacing with normal rehab, and see if patients who've been through all of their other usual therapies after a stroke can get even better.
According to the University, volunteers in the study undergo three 1-hour sessions of "intensive physiotherapy" per week for a total of six weeks. In addition, half of those volunteers also receive stimulation with Vivistim, which works by stimulating the nerve when an exercise is performed correctly. This helps train the brain to remember that particular movement.
The device builds on existing research that show vagus nerve stimulation potentially prompting the brain to release neurotransmitters that aid in forming new neural connections. This process may help restore function to, for example, a limb affected by the stroke.
SOURCE: Ohio State University