Biomedical Parts Created Using New Cold Spray 3D Printing Process
Researchers led by scientists from Cornell have developed a new 3D printing technique that creates cellular metallic materials using a unique process that smashes powder particles together at supersonic speeds. The technology is known as "cold spray" and creates a mechanically robust and porous structure 40 percent stronger than similar material made with conventional manufacturing processes. The small size of the structures and porosity makes them well suited to build biomedical components, like replacement joints.
The lead author of the research paper is Atieh Moridi. He says that the cellular structures the team focused on have applications in thermal management, energy absorption, and biomedicine. Rather than using heat as the driving force behind bonding, the new technique uses plastic deformation to bond the powder particles together. Rather than carving a shape out of a large block of material, the additive manufacturing technique used here builds the product layer by layer.
One downside of additive manufacturing is that typically metallic materials have to be heated at high temperatures to exceed their melting point resulting in residual stress build-up, distortions, and unwanted phase transformation. Researchers developed their new method to eliminate those issues using a nozzle of compressed gas to fire titanium alloy particles at a substrate.
Particles used in the process are between 45 and 106 microns in diameter and travel at about 600 meters per second. The team notes that they don't simply hurl metallic particles as fast as possible. They had to carefully calibrate the titanium alloy's ideal speed. The team determined the speed that was just under the alloy particle's critical velocity.
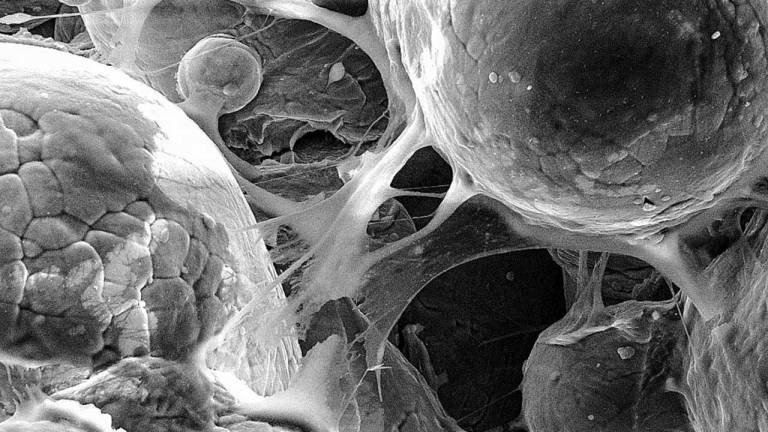
The particles launched at that rate create a more porous structure ideal for biomedical applications, such as artificial joints and cranial or facial implants. The team says that these porous constructions allow the bone to grow inside the pores to create a biological fixation. That reduces the likelihood of the implant becoming loose and causing pain.